Menopause and Incontinence: What You Should Know2 Comments20 April 2023 Last Updated: 13 July 2024 Menopause is a natural phase in a woman's life that marks the end of her reproductive years. It is a time when our bodies undergo hormonal changes, including a decrease in oestrogen levels, which can effect woman's health. Symptoms include hot flushes, night sweats, vaginal dryness, mood changes, sleep problems and weight gain. The menopausal years can span any time from 45-55 years. Some women who go through an early menopause could experience symptoms of menopause such as night sweats of hot flushes at a much younger age. In the UK, the average age is 51. But around one in 100 women experience the menopause before 40 years of age. There are three main phases of menopause: - Perimenopause: The transitional period leading up to menopause, where hormone levels fluctuate and menstrual cycles become irregular. This phase can last several years.
- Menopause: The point at which a woman has not had a period for 12 consecutive months.
- Post-menopause: The years following menopause.
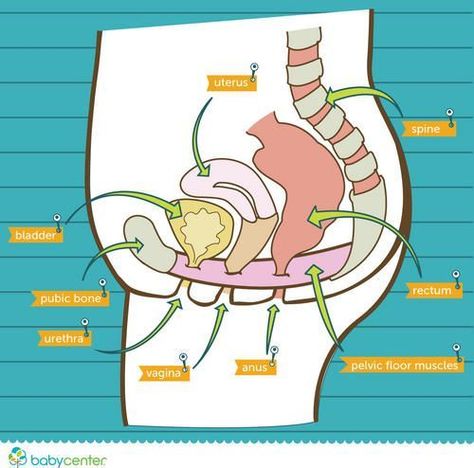
At Cheeky Wipes HQ, we are mostly in the 45 to 50 age bracket and feeling the full effects of perimenopause which can occur for many years while still having our monthly cycles. Joy! One common issue that many women experience during menopause is incontinence, or the involuntary loss of urine. In this blog post, we will look at the link between menopause and bladder weakness, including why it happens, what the common symptoms are, and how can it be managed. Can Menopause Cause Incontinence? Incontinence, the involuntary loss of urine, can be a symptom of menopause. Oestrogen levels decrease during menopause, which can affect the pelvic floor muscles as these muscles provide support for the bladder and urethra. Postmenopausal women may find muscles become weaker, leading to problems with bladder control. This condition can be distressing and affect your quality of life. Let's look at this on more detail... What Are Pelvic Floor Muscles and Why Are They Important?Your pelvic floor muscles are a broad sling of muscles, like a trampoline, stretching from your pubic bone at the front of your pelvis to your coccyx (tail bone) at the back. They form the floor of your pelvis and are responsible for: - Supporting your pelvic organs – your bladder, bowel and womb.
- Controlling your bladder, bowel and sexual functions.
Why Does Menopause Cause Incontinence?
Oestrogen levels are important for maintaining the health and strength of your pelvic floor muscles. Reduced levels of oestrogen starting around menopause can cause thinning of the lining of the urethra, the short tube that passes urine from the bladder, which can cause leaks. In addition, the surrounding bladder and pelvic floor muscles also may weaken with ageing, a process known as pelvic relaxation. As a result, the pelvic floor muscles may not be able to effectively support the bladder and urethra. Women at midlife and beyond are at increased risk, or an exacerbation of pre-existing, stress and urge incontinence. Pelvic floor stress incontinence is the most common form of incontinence. It is caused by weakened pelvic floor muscles and means you leak urine when you increase pressure on the bladder such as when coughing and sneezing or during exercise. As it is caused by weakness, the main treatment for pelvic floor stress incontinence is to strengthen your pelvic floor muscles with pelvic floor training - in fact around 60% of cases cure or are dramatically improved by exercise alone. Menopause Incontinence SymptomsThe types of urinary incontinence and most common symptoms of bladder weakness during menopause may include: - Overflow incontinence - Pee leaks when coughing, laughing, sneezing, or lifting.
- Urge incontinence - Frequent and sudden urges to urinate.
- Difficulty holding urine for long periods of time.
- Needing to use the toilet more frequently, including during the night.
- The feeling of a constant urgency to urinate.
How to Manage Incontinence During MenopauseIf you are experiencing incontinence during menopause, there are several strategies you can try to manage it effectively. Here are some suggestions: 1. Pelvic Floor ExercisesPelvic floor strength can be improved by training your pelvic floor muscles. To strengthen the muscles, you should imagine you are having a wee and trying to stop the flow of urine. Once you are confident you are using the right muscles you should aim to hold for 5 seconds, relax and repeat 10 times - these are also known as 'slow' Kegel exercises. Then using the same principle, engage your pelvic floor muscles and hold for just 2 seconds, relaxing and repeating 10 times; these are called ‘fast' Kegels exercises. Aim to repeat the process of fast and slow Kegels for 5 minutes or 10 sets and do this minimum of three times a day. As you become stronger you can increase the hold of the ‘slow Kegels’ to 10 seconds. Regular practice can help improve bladder control. You can learn how to do these exercises from a nurse or a physio specialising in pelvic floor health. Or do it yourself with the help of a pelvic floor trainer, which can improve your results: - Kegel Weights: These weighted balls are inserted into the vagina and held in place by contracting the pelvic floor muscles. The weight and movement encourage the muscles to work harder, strengthening them over time.
- Electrical Stimulation Devices: These devices use gentle electrical impulses to stimulate the pelvic floor muscles, causing them to contract and strengthen over time. They are particularly useful for individuals who have difficulty identifying or contracting their pelvic floor muscles on their own.
- Biofeedback Devices: These devices provide real-time feedback on muscle activity. They often connect to an app or display that shows the strength and duration of muscle contractions, helping users ensure they are performing the right exercises.

2. Bladder TrainingSchedule regular bathroom visits and gradually increase the intervals between them to train the bladder to hold urine for longer periods. This can improve bladder control and reduce the frequency of urgent urination. Experts recommend that you: - Empty your bladder as soon as you get up in the morning. This act starts your retraining schedule.
- Go to the bathroom at specific times. Wait until your next scheduled time before you urinate again. Be sure to empty your bladder even if you feel no urge to urinate.
- When you feel the urge to urinate before the next designated time, use "urge suppression" techniques or try relaxation technique.
3. Wear Incontinence ProtectionUsing reusable incontinence pads or washable pants can help manage leaks and provide peace of mind. There are various types and styles available that are discreet and comfortable. Opting for reusable products such as reusable knickers and pads can help reduce costs. You won't run out, and they are much more gentle on sensitive skin. Need helping finding the right product? Read our guide on the best incontinence underwear for women. 
4. Avoid Caffeine and AlcoholBoth can irritate the bladder, leading to more frequent urination and a higher chance of leaks. Limiting or avoiding these substances may help reduce symptoms. On a similar note, drinking adequate water to stay hydrated is essential, but it's also important to avoid drinking large amounts of fluids at once. 5. Seek Medical AdviceIf you are experiencing incontinence during menopause, it's important to talk to a Doctor. Your GP can assess the intensity of your symptoms, identify the source of the problem and suggest the best treatment plan for you, such as: - Medications: Various medications can help manage symptoms of an overactive bladder and stress incontinence.
- Hormone Replacement Therapy (HRT): While HRT can help alleviate some menopausal symptoms, its role in treating incontinence is still being studied.
- Surgery: In severe cases, surgical options like bladder sling procedures can provide relief from stress incontinence.
Incontinence can be a common symptom experienced during menopause due to hormonal changes that affect the pelvic floor muscles. For many people, this can be distressing and affect quality of life - in particular outside of the house, such as in work. However, there are strategies that can help manage incontinence effectively. Pelvic floor exercises, using incontinence protection, avoiding bladder irritants, bladder training, and seeking medical advice can all help. Remember that you are not alone, and it's important to talk to someone for individual guidance on managing incontinence during menopause. "I went through an early menopause at 33, so don't need the pants and pads for periods anymore. I've bought various products over this past year and have found everything fantastic, both for the description and other ways to use them. The period and pee pants saved my clothes and carpets last week as I wanted to watch the end of a film before I went toilet. Obviously I'd left it a little late and as I hobbled up the stairs the floodgates open and by the time I got there, I'd emptied most of my bladder lol. My clothes (other than the pants) were all dry so I'm amazed at how much liquid they held. I use the baby wipes to clean things and any of the other products everywhere around my house. I love these products so much" Helen Nov '22 Trustpilot If you found this blog useful you may like - When to change your incontinence pads or pants Best incontinence pads for sensitive skin Incontinence pants V's Pads : all you need to know Can you use incontinence underwear for periods? You can browse all our blogs here. As always, if you're unsure of what you need to make the switch to reusable sanitary products and period pads, please do drop the team a line or use the online chat function. The team all use the products themselves and just LOVE to chat pee poo and periods, all day long, nothing is TMI and we all love to overshare based on our own experiences... About the Author: Kirstin Scriven is part of the Customer Experience team at Cheeky Wipes, which since 2008 has been selling the original reusable wipes kit. She is mum to 3 and loves the forest, the sea and the hills! Along with the rest of our crack team, she spends most days talking about poo, pee and periods and loves a chance to overshare. The business was recognised with a Queens Award for Enterprise in Sustainable Development in 2021, celebrating their hard work over the last 13 years. |
Hi, I am perimenopausal cheerleader 47yrs size 16 tight kit is tight leggings, that has sudden incontinent leeks when lifting and catching fellow athletes. I have a competition coming up and fear my pad isn't good enough what would u suggest?
Hi Sally, Cheerleading sounds awesome! I'd recommend our heaviest absorbency pant for you Feeling Fearless bamboo or Feeling Free leopard print or our organic night pad, I'll pop some links here but feel free to email into us at customers@cheekywipes.com to discuss further,
https://www.cheekypants.com/high-waisted-period-pants/feeling-fearless-bamboo-high-waist-period-pants-heavy-flow.html
https://www.cheekypants.com/boybrief-period-pants/feeling-free-boybrief-style-mid-rise-period-pants-organic-cotton-prints.html
https://www.cheekypants.com/cotton-cloth-sanitary-pads/cheeky-pads-organic-cotton-cloth-period-nightmaternity-pad-standard.html
Best wishes,
Kirstin